Great article by Dr Weber and Panaxea.
The levels of different molecules within tumour cells yield information about cancers nature and in breast cancer, one of the most crucial for helping guide treatment is the oestrogen receptor (ER). Women with high levels of this molecule in their cancer cells (called ER-positive breast cancer) benefit from hormone therapy drugs that either lower their oestrogen levels, or prevent cancer cells responding to the hormone. About 7 out of ten women have ER-positive breast cancer.
ER-positive Breast Cancer.
But theres a second molecule the progesterone receptor (PR) levels of which inside breast cancer cells also seem to be important. Doctors have known for a long time that women with high levels of both the oestrogen and progesterone receptors (double-positive) have the best chance of surviving they respond better to treatment, and their cancer is less likely to spread. But these double-positive women are given the same hormone therapy as those who have no progesterone receptor in their breast cancer, so doctors dont always routinely test for this second molecule any more.
Until now, its been unclear why having high levels of both molecules is good news for the patient, or what benefit testing for progesterone brings.
But thanks to Cambridge-based Cancer Research UK researcher Dr Jason Carroll and his team, and their colleagues at the University of Adelaide in Australia, there are finally answers to this mystery. Today, theyve published surprising results of a study in the journal Nature that finally solves the puzzle of why double-positive women do better. And if their findings are confirmed in follow-up studies, it could make a big difference to how women are treated.
How do the ER and PR receptors work?
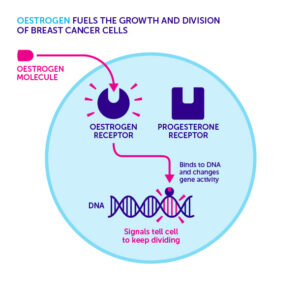
Only certain types of cells that respond to hormones make these receptors for example breast, ovary and womb cells. Both receptors are directly involved in switching genes on and off theyre called transcription factors. When oestrogen and progesterone are present, these hormones physically stick to their respective receptor, causing them to move into the nucleus of the cell, where DNA is housed. They can then attach to specific regions of our DNA and turn genes on or off, changing the cells behavior. When breast cancer develops, the tumour cells become overly sensitive to oestrogen. When oestrogen activates the oestrogen receptor, it turns on a panel of genes that tell the cells to keep dividing, driving tumour growth:
But what happens when breast cancer cells have a working progesterone receptor too?
The first piece of the jigsaw fell into place when they looked at the physical relationship between the two receptors. Using double-positive breast cancer cells grown in the lab, they made sure the cells had sufficient oestrogen and progesterone to activate both receptors, then they cracked the cells open.
When they used a sophisticated method to fish out the progesterone receptor from the resulting mixture, they discovered something unexpected: it was physically stuck to the oestrogen receptor. This was a strong hint that progesterone via the progesterone receptor was somehow affecting how the oestrogen receptor works.
Using the same lab-grown breast cancer cells exposed to oestrogen only, the researchers used cutting-edge technology to pinpoint the sites in the cells DNA where activated oestrogen receptor attached hence which genes it was controlling.
But when the scientists then added progesterone to the cells too, it caused a rapid shift in the points where oestrogen receptor attached to DNA.
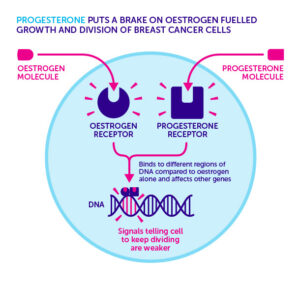 At least 470 genes were controlled differently when both hormones were present compared to just oestrogen alone the progesterone receptor was, in effect, reprogramming the oestrogen receptor, changing the genes that it influences.
At least 470 genes were controlled differently when both hormones were present compared to just oestrogen alone the progesterone receptor was, in effect, reprogramming the oestrogen receptor, changing the genes that it influences.
But, most crucial part was the overall effect this on the cancer cells themselves progesterone seemed to cause the cells to stop growing as quickly.
By changing the genetic programme, the progesterone receptor was applying the brakes to the cells growth.
The cells used in the above experiments are based on tissue samples taken many decades ago, and kept artificially growing in a lab (called cell lines). These are a good starting point, but it was important to show this ER reprogramming actually happens in human disease.
So the team turned a special technique developed by scientists in Professor Wayne Tilleys laboratory at the University of Adelaide in Australia. This allowed small samples of tumour tissue to be removed from women with breast cancer and grown in the lab for a short time. Remarkably, the team saw exactly the same effect adding progesterone at the same time as oestrogen slowed down the rate tumours grew.
They also saw exactly the same phenomenon in mice transplanted with human breast cancer cells: oestrogen fuelled tumours growth, but progesterone put the brakes back on. The final, and most crucial, experiment was to see if their findings had any potential implications for treating breast cancer. Again working with mice transplanted with tumour samples and given oestrogen, the researchers used the standard treatment for hormone-responsive breast cancer tamoxifen, which slowed down tumour growth.
But when they gave the mice tamoxifen AND progesterone, the tumours grew even more slowly. Changing the way breast cancer is treated? Dr Carrolls research is a big step forward in understanding the role of progesterone receptor in breast cancer. Until now, its presence was simply considered an indication of how good a womans chances of surviving were. But Dr Carrolls study findings reveal that the receptor itself is the direct reason why these women have a better outlook. Understanding the progesterone receptors role as a molecular handbrake on oestrogen-fuelled growth could also explain the observation that breast cancers frequently evolve to get rid of their progesterone receptors this is an advantage to cancer, helping it grow quicker. This new research offers a unique opportunity to exploit the braking action of the receptor with hormone therapy to improve breast cancer outcomes. According to Dr Carroll, this is precisely what needs to be done, and the next steps are obvious. The results are pretty clear and potentially have direct benefits for many women with breast cancer, he told us.
Were already discussing a clinical trial to test whether giving women with ER/PR double-positive breast cancer progesterone, alongside oestrogen-blocking drugs, helps more women survive this disease. If proven successful, they suggest that it could benefit up to half of women diagnosed with the disease.